Pregnant...on birth control?
And the news about the CDC pregnancy research experts getting fired. Cool.
I look forward to the day when the news I share in this newsletter is positive! But unfortunately, today is not that day. My goal isn’t to depress you, though; rather, I am trying to inform you and give you actionable ways to fight back if you feel you want to (and I hope you do!). So with that in mind, thanks for reading. -Dr. Jen
In the News: CDC cuts will hurt kids, parents, and parents-to-be
Big news hits this week: Federal budget cuts have gutted key maternal, newborn, and fertility health programs, and even led to layoffs of the CDC experts who’ve long protected families across the country.
Here’s what’s at risk:
Trump’s proposed cuts include eliminating the federal Department of Reproductive Health, which helps guide policy and protections for fertility care like IVF. Without this, access to IVF could become more limited and vulnerable to state-level restrictions.
Newborn hearing screenings could be rolled back as the CDC’s Early Hearing Detection and Intervention program loses staff and support.
Maternal health tracking is in danger, with the Pregnancy Risk Assessment Monitoring System (PRAMS) losing funding in multiple states. This is a CDC program that collects state-specific data on maternal experiences and health before, during, and shortly after pregnancy to help improve outcomes for mothers and babies. It’s basically the most trusted data set we have on pregnancy health in the United States—and now it’s being gutted.
Progress on genetic screening for newborns is stalling after the shutdown of the Advisory Committee on Heritable Disorders.
And perhaps most alarming: the CDC professionals behind many of these programs were fired—leaving fewer public health experts to watch out for women and babies.
The bottom line: This isn’t about efficiency—they’re cuts that will have real, long-term impacts on maternal mortality, infant health, and access to fertility care.
What You Can Do
Speak up!
Use the Five Calls app (or visit 5calls.org) to find your elected officials and make your voice heard in under 5 minutes. They even provide phone numbers and talking points.
Here’s a script you can use when you make the call:
Hi, my name is [Your Name], and I’m a constituent of [Name of Representative]. I’m calling because I’m deeply concerned about recent federal cuts to maternal health programs, newborn screening, and IVF protections. These services are essential for families and should not be on the chopping block. I’m asking you to protect funding for CDC programs like Early Hearing Detection and Intervention and the Pregnancy Risk Assessment Monitoring System, and to support legislation that ensures access to safe, affordable fertility care. Thank you.
Every call truly counts—and yours could help preserve these life-saving programs for millions of families.
Q&A: Pregnant on the pill!
Q: I just found out I got pregnant while on the birth control pill. I know it’s not 100% effective but this is a shock. Now that we’ve decided to keep the pregnancy, I’m worried the pill may have harmed the baby. Could the hormones in the pill harm raise the risk of miscarriage or affect any development?
A: You are definitely not alone in this experience—but I am sorry about the stress it has caused. Birth control pills are very effective when taken consistently and correctly, but they’re not perfect. With typical use, about 7 out of 100 people will become pregnant within a year. Over time, those odds add up—so it’s not uncommon to see pregnancies happen even in people who’ve been using the pill for years. In fact, scroll down to this week’s resource to visually see just how common this is!
The good news: if you’ve just found out you’re pregnant and were still taking the pill at the time, there is no strong evidence that this will harm your baby. Research has not shown any increased risk of birth defects, miscarriage, or developmental problems from hormone exposure early in pregnancy.
Want to get your question answered in the BBC newsletter? Shoot me a message and I’ll incorporate them into future newsletters!
*no personalized medical advice*
Resource of the week: the New York Times?!
Why am I sharing this article from the New York Times? From all the way back in 2014??
Because it’s one of my faves, that’s why! It explains birth control failure —aka how likely are you to get pregnant while using a certain method—in such a visual, usable way.
Just like the person asking this week’s question, you can get pregnant on birth control. And while we often tell people how likely this is, what does a 93% failure rate really mean?
Let’s me show you:
Take the birth control pill. With typical use (which is what we’ll go by as opposed to perfect use, because in reality people aren’t perfect!), the failure rate is 93%. That means in 1 year of women having vaginal sex using the birth control pill, 7 out of 100 will get pregnant. That makes sense, right? And you can see that in this interactive graph from the NYT article below (though they say it has a failure rate of 91%, so let’s just go with that here):

Here’s why I love this graph. It truly shows how the probability of pregnancy increases over time. As they explain, this is “the same way that any small risk, taken repeatedly, grows in likelihood.” So here’s your pregnancy chances at five years on the pill:

And then I think the most sobering of all…ten years:
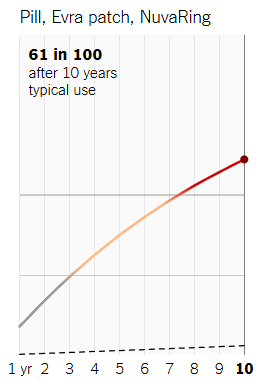
So yes: If the same group of 100 women use the birth control pill for 10 years and are having sex, 61 of them will become pregnant. That sure sounds different than a 93% effectiveness rate, right?!
I share this not to scare you, but to help you when choosing a birth control method because if you don’t want to become pregnant seeing the risks this way makes it much easier to see what you might want to use (and what you might want to avoid).
For example, if not getting pregnant is the most important aspect of picking a birth control method (it’s not always for everyone, and that’s OK), you can see how methods like the IUD or arm implant (Nexplanon might be more desirable. Look how well they work even at 10 years:

OK - heavy week, but lots of ways we can speak up, advocate, and take control of our own reproductive health by knowing what we need to stay safe and protected. Please share these resources with those in your community—it really does take a village.
Until next time,
Dr. Jen




